As posted on diabeticfootonline.com by David G. Armstrong
A recent meta-analysis, published in Wound Repair and Regeneration, systematically examined healing rates for diabetic neuropathic foot ulcers (DFUs) in patients receiving standard-of-care treatments. The study, led by Tyler Coye and a distinguished group of co-authors, including long-time research partner Lawrence A. Lavery, underscores a critical need for improved strategies in DFU management.
Key Findings
The analysis synthesized data from 32 randomized controlled trials (RCTs) conducted over nearly three decades (1996–2023). In total, the trials encompassed sample sizes ranging from 9 to 169 patients, providing a comprehensive view of DFU healing outcomes under current standard-of-care treatments.
• Healing Rates:
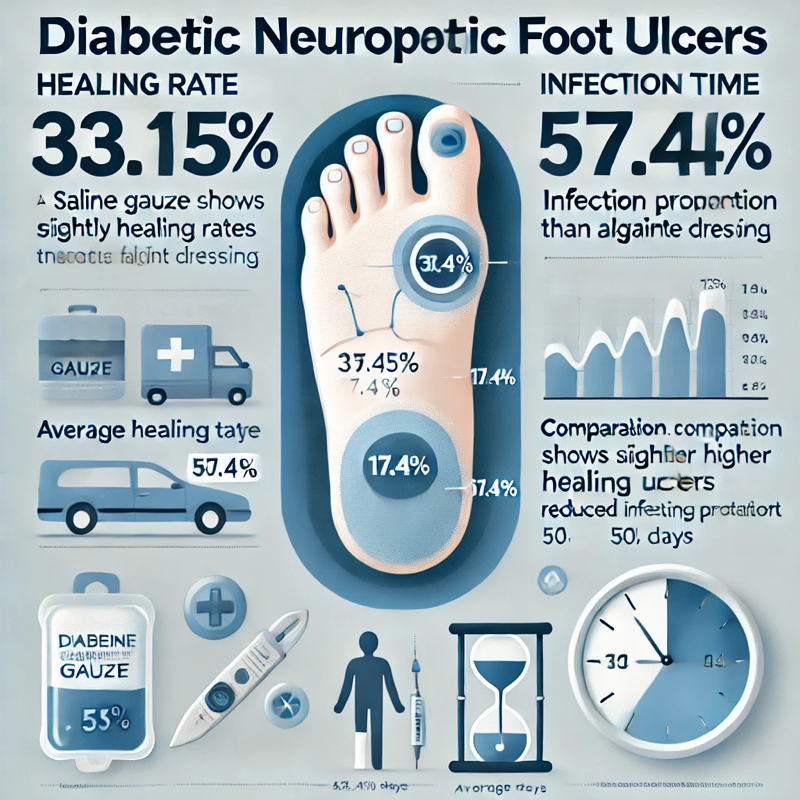
The pooled healing rate within a 12- to 24-week treatment period was 33.15% (95% CI: 31.18%–35.11%), meaning only about one-third of patients achieved complete wound closure.
• Healing Time:
The average healing time was approximately 50.14 days, with a standard deviation of 31.10 days.
• Infection Proportion:
Despite standard care, the pooled infection proportion was notable at 17.4% (95% CI: 12.2%–22.5%).
• Treatment Comparisons:
Subgroup analysis revealed that healing rates were marginally better with saline gauze compared to alginate dressings, although alginate demonstrated a reduced infection proportion.
• Study Robustness:
Sensitivity analyses affirmed the robustness of the findings, but the presence of publication bias, as detected by Egger’s test, necessitates cautious interpretation.
Why This Matters
Diabetic foot ulcers remain one of the most challenging complications of diabetes, often leading to severe consequences such as infection, hospitalization, and amputation. Despite the widespread implementation of standard-of-care treatments, the results from this meta-analysis highlight their limited effectiveness in achieving consistent wound healing.
The significant variability (heterogeneity) observed among trials also suggests a pressing need for:
• Advanced wound care strategies beyond conventional therapies.
• Personalized treatment plans to address patient-specific needs and improve outcomes.
• High-quality, well-reported randomized controlled trials to better identify effective interventions for DFUs.
A Call for Innovation
This research underscores the vital need to push the boundaries of DFU care through novel approaches and technologies. Advanced therapies, such as bioengineered tissue, growth factors, and smart wound monitoring systems, hold potential for improving outcomes in ways that standard treatments have not.
Gratitude to the Authors
We extend our appreciation to Lawrence A. Lavery, a long-time leader in DFU research and a collaborator whose work has shaped our understanding of diabetic wound healing. This study, conducted alongside a talented team of co-authors, reinforces the importance of continued innovation and evidence-based care in managing diabetic foot ulcers.
Reference:
Coye TL, Bargas Ochoa M, Zulbaran-Rojas A, et al. “Healing of diabetic neuropathic foot ulcers receiving standard treatment in randomised controlled trials: A random effects meta-analysis.” Wound Repair Regen. 2025;33(1):e13237. DOI: 10.1111/wrr.13237.

